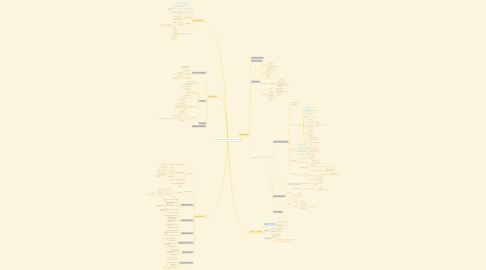
1. Thyroglossal cyst
1.1. painless, soft, round lump in the front center of the neck.
1.2. typically move when the person swallows or sticks their tongue out.
1.3. Surgical removal of the cysts
1.3.1. helps prevent recurrence and infection.
1.4. may have no symptoms at all and can go unnoticed until they become infected.
1.5. Diagnostic tests
1.5.1. blood test
1.5.2. ultrasound examination
1.5.3. fine needle aspiration
1.5.4. X-rays with a contrast dye
1.6. Treatment
1.6.1. Surgery is a standard treatment option
1.6.2. Sistrunk procedure
1.6.2.1. is the most effective in removing thyroglossal cysts so that they do not reoccur.
1.7. omplications after surgery
1.7.1. Bleeding
1.7.2. Clotting
1.7.3. Fistula
1.7.4. Infection
1.7.5. Scarring
1.7.6. Nerve damage
1.7.7. Hypothyroidism
2. Types of biopsy
2.1. Fine Needle Aspiration Cytology (FNAC)
2.1.1. The best initial test to diagnose a neck mass.
2.1.2. Gives cellular result
2.1.3. Often done in clinic. No need for anaesthesia
2.2. Core Biopsy
2.2.1. be done instead of or after an FNAC to confirm the findings by tissue diagnosis .
2.2.2. slightly larger needle and gets a piece of tissue.
2.3. An open biopsy
2.3.1. more invasive procedure.
2.3.2. Done in the operating room
2.3.3. Need anesthesia.
2.3.4. Type
2.3.4.1. A. Incisional biopsy
2.3.4.1.1. üRemove only portion of the mass
2.3.4.2. B. Excisional biopsy
2.3.4.2.1. Remove the whole mass.
3. Thyroid cancers
3.1. Epidemiology
3.1.1. Commonest endocrine malignancy
3.1.1.1. 1% of all malignancies
3.1.1.2. 0.5-1 per 100000
3.1.2. Good prognosis
3.1.2.1. Papillary Ca
3.1.2.1.1. 74-93% long-term survival rate
3.1.2.2. Follicular Ca
3.1.2.2.1. 43-94% long-term survival rate
3.1.2.3. Hurthle Cell Ca
3.1.2.3.1. 20% mortality rate at 10 years
3.1.2.4. Medullary Ca
3.1.2.4.1. 80% 10-year survival rate 45% with LN involvement
3.1.2.5. Anaplastic tumour
3.1.2.5.1. Median survival of 4-5 months at time of diagnosis
3.1.3. Annual Incidence
3.1.3.1. 3.7 per 100,000
3.1.4. Sex
3.1.4.1. Female
3.1.5. Can occur at any age group
3.2. Thyroid Neoplasm
3.2.1. Benign
3.2.2. Malignant
3.2.2.1. Primary
3.2.2.1.1. Lymphoid Cells
3.2.2.1.2. Parafollicular Cells
3.2.2.1.3. Follicular Cells
3.2.2.2. Secondary
3.3. Papillary Carcinoma
3.3.1. Most common Thyroid carcinoma (80%)
3.3.2. Slow growing painless mass. Euthyroid-status.
3.3.3. LN metastases is common, may be the presenting symptom.
3.3.4. Distant metastases is uncommon at initial presentation.
3.4. Follicular Carcinoma
3.4.1. 10% of all thyroid cancers.
3.4.2. common in Iodin-deficient areas.
3.4.3. rapid increase in size and long-standing goiter.
3.4.4. Cervical LN metastasis is uncommon.
3.4.5. distant metastasis may be present.
3.4.6. Spread by blood vessels
3.5. Medullary Carcinoma
3.5.1. 5% of all thyroid malignancies.
3.5.2. Most cases are sporadic, 25% are inherited.
3.5.3. Local pain or aching is common.
3.6. Anaplastic Carcinoma
3.6.1. 1% of all thyroid malignancies.
3.6.2. More in Women
3.6.3. LN are usually involved at presentation.
3.6.4. ± Distant metastasis.
3.7. Thyroid lymphoma
3.7.1. 1% of all Thyroid Ca.
3.7.2. Most are Non-Hodgkin B-cell Lymphoma.
3.7.3. FNAC is diagnostic.
3.8. Hurthle-Cell Carcinoma
3.8.1. 3% of all Thyroid Ca.
3.8.2. Subtype of Follicular Ca.
3.8.3. FNAC is not conclusive.
3.8.4. Lobectomy + isthmusectomy
3.8.4.1. unilateral
3.8.5. Total Thyroidectomy
3.8.5.1. bilateral
4. Hyperthyroidism
4.1. Toxic thyroid nodule.
4.2. Iatrogenic (drugs).
4.3. Thyroid storm.
4.3.1. Cause
4.3.1.1. Inadequately treated thyrotoxicosis.
4.3.1.2. Following subtotal thyroidectomy/radio active iodine.
4.3.2. Signs
4.3.2.1. Elevation of temperature.
4.3.2.2. Increase in heart rate.
4.3.2.3. Irritable.
4.3.2.4. Comatose
4.3.2.5. Vomiting
4.3.2.6. Diarrhea
4.3.3. Emergency management
4.3.3.1. Administer oxygen.
4.3.3.2. Monitor all vital signs.
4.3.3.3. Start IV line with drip of crystalloid solution(150mL/hr).
4.3.3.4. Transport patient to emergency care facility.
4.3.4. Management
4.3.4.1. Propranolol
4.3.4.1.1. 80mg/6hrs orally(dose of 1-5mg/6hrs given IV).
4.3.4.2. Potassium iodide
4.3.4.2.1. 60mg daily orally/ sodium iopodate 500mg daily orally.
4.3.4.3. Carbimazole
4.3.4.3.1. 60-120mg daily
4.3.4.4. Dexamethasone
4.3.4.4.1. 2mg/6hrs IV.
4.3.4.5. Fluid replacement.
4.3.4.6. Antibiotics.
4.4. THYROTOXICOSIS
4.4.1. Hyper metabolic , serum elevation of thyroid hormone
4.4.1.1. Grave’s disease (primary)
4.4.1.1.1. Autoimmune disease.
4.4.1.1.2. More On Female
4.4.1.1.3. Signs and symptoms.
4.4.1.1.4. Eye signs
4.4.1.1.5. Investigations
4.4.1.1.6. Management
4.4.1.2. Multi-nodular goiter
4.4.1.2.1. Excess production of thyroid hormones from functionally autonomous thyroid nodules
4.4.1.2.2. Symptoms
4.4.1.2.3. Management
4.4.1.3. Toxic adenoma.
5. Hypothyroidism
5.1. Hashimotos thyroiditis.
5.1.1. Primary condition of hypothyroidism
5.1.2. Autoimmune
5.1.3. Diagnosis
5.1.3.1. T3 & T4 levels.
5.1.3.2. Presence of TPO antibodies.
5.1.4. Treatment
5.1.4.1. Thyroxin therapy.
5.1.4.2. Helps in both hypothyroidism and goiter shrinkage
5.2. Cretinism.
5.2.1. dating from birth.
5.2.2. Earlier onset greater is the brain damage.
5.2.3. Causes
5.2.3.1. Congenital developmental defects.
5.2.3.2. Radio iodine/surgery.
5.2.3.3. Post radiation.
5.2.3.4. Iodine deficiency.
5.2.3.5. Drug induced.
5.2.3.6. Hashimoto’s thyroiditis.
5.2.3.7. Recurrent hypothyroidism.
5.2.4. Signs and symptoms
5.2.4.1. Dry, cool, mottled skin
5.2.4.2. hoarse cry
5.2.4.3. broad flat nose+puffy face.
5.2.4.4. Protuberant abdomen, umbilical hernia, hypotonia.
5.2.4.5. Lethargy, poor feeding/sucking.
5.2.4.6. Cold to touch.
5.2.4.7. Delayed dentition.
5.2.4.8. Mental retardation.
5.2.5. Management
5.2.5.1. Investigation
5.2.5.1.1. Cord blood T4, TSH , Serum T4, TSH
5.2.5.2. Treatment
5.2.5.2.1. Medication
5.2.5.3. Diet
5.2.5.3.1. iodine rich foods
