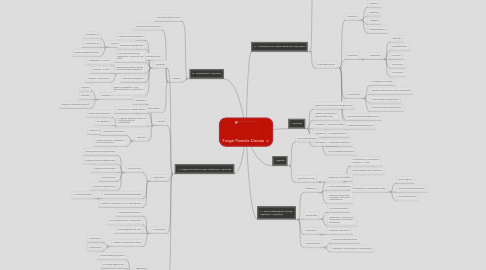
1. B. Superficial Mycoses
1.1. acquired by direct contact
1.2. diseases
1.2.1. Black piedra & white piedra
1.2.2. dermatophytoses
1.2.2.1. 3 genera of Ascomycetes
1.2.2.1.1. Tricophyton sp
1.2.2.1.2. Microsporum sp
1.2.2.1.3. Epidermophyton floccosum
1.2.2.2. Classification
1.2.2.2.1. Anthopophilic - humans
1.2.2.2.2. Zoophilic - animals
1.2.2.2.3. Geophilic - soil (invasive)
1.2.3. Malassezia infection
1.2.3.1. Malassezia furfur (basidiomycetes)
1.2.3.1.1. pityriasis
1.2.3.1.2. folliculitis
1.2.3.1.3. seborrheic dermatitis (dandruff)
1.2.3.2. Treatment
1.2.3.2.1. ketoconazole shampoos
1.2.3.2.2. zinc pyrithione
1.2.3.2.3. selenium sulfide lotions
2. A. Opportunistic Fungi: Systemic Mycoses
2.1. Aspergillus
2.1.1. Hypersensitivity aspergillosis
2.1.2. Noninvasive aspergillomas
2.1.3. Acute invasive pulmonary aspergillosis - necrosis of lung tissue
2.1.4. Nonpulmonary disease (severe than pulmonary aspergillosis)
2.1.5. Cutaneous aspergillosis
2.1.6. Systemic aspergillosis - high dose intravenous of Amphotericin B
2.2. Candida
2.2.1. Candidiasis
2.2.2. Most Common: Candida albicans
2.2.3. Diagnose: signs and clusters of budding yeast and psedohyphae
2.2.4. Treatment
2.2.4.1. AIDS patient: fluconazole
2.2.4.2. Invasive candiasis: Amphotericin B & 5-fluorocytosine
2.3. Cryptococcus
2.3.1. Cryptococcosis
2.3.1.1. primary pulmonary cryptococcosis
2.3.1.2. Invasive pulmonary cryptococcosis
2.3.1.3. Cryptococcal meningitis
2.3.1.4. Cryptococcoma
2.3.1.5. Cutaneous cryptococcosis
2.3.2. Crptococcus neoformans (Basidiomycetes)
2.3.2.1. C. neoformans gattii
2.3.3. Treatment: Amphotericin B + 5-fluorocytosine
2.4. Pneumocystis
2.4.1. Pneumocystis Pneumonia
2.4.2. Pneumocystis jiroveci - Ascomycetes
2.4.3. Almost diagnostic with Aids
2.4.4. Treatment: Antiprotozoan drugs
2.4.4.1. Trimethoprim
2.4.4.2. Sulfanilamide
2.5. Mucor
2.5.1. Zygomycosis
2.5.1.1. Rhinocerebral zygomycosis
2.5.1.2. Pulmonary zygomycosis
2.5.1.3. Gastrointestinal zygomycosis
2.5.1.4. Cutaneous zygomycosis
2.5.2. mucor, rhizopus & absidia - Zygomycota
2.5.3. Treatment: remove infected tissue with Amphotericin B
3. Mycoses
3.1. Systemic Mycoses due to pathogenic fungi
3.2. Systemic Mycoses due to Opportunistic Fungi
3.3. Superficial Mycoses
3.4. Cutaneous Mycoses
3.5. Subcutaneous Mycoses
4. Agents
4.1. True Fungal Pathogen
4.1.1. Blastomyces dermatitidis
4.1.2. Coccidioides immitis
4.1.3. Histoplasma capsulatum
4.1.4. Para coccidioides brasiliensis
4.2. Opportunistic Fungi
4.2.1. Dermatophytes
4.2.1.1. Microsporum sp: Microsporum audouiinii, M. Canis
4.2.1.2. Epidermophyton sp: E. floccosum
4.2.1.3. Trichophyton sp: Trichophyton rubrum
4.2.1.3.1. Tinea incognito
4.2.1.3.2. Tinea of nails (onychomycosis)
4.2.1.3.3. Tinea barbae: beard
5. A. True Pathogenic Fungi: Systemic Mycoses
5.1. Blastomyces
5.1.1. Blastomyces dermatitidis
5.1.2. Pulmonary Blastomycosis
5.1.3. Treatment: Itraconazole, Fluconazole, Ketonazole, Amphotericin B.
5.2. Coccidioides
5.2.1. Coccidioides immitis
5.2.2. Treatement: Amphotericin B, Ketoconazole, Fluconazole, Itraconazole
5.3. Histoplasma
5.3.1. Histoplasma capsulatum
5.4. Paracoccidioides
5.4.1. Paracoccidioides brasiliensis
5.4.2. Treatement: Amphotericin B or ketoconazole
6. C. Cutaneous & Subcutaneous Mycoses
6.1. Chromoblastomycosis
6.1.1. Fonsecaea pedrosoi
6.1.2. F. compacta
6.1.3. Phialophora verrucosa
6.1.4. Cladophilophora carrionii
6.2. Phaeohyphomycosis
6.2.1. Caused by:
6.2.1.1. Alternaria
6.2.1.2. Exophiaca
6.2.1.3. Wangiella
6.2.1.4. Cladophialophora
6.2.2. Mycetomas
6.2.2.1. Ascomycota
6.2.2.1.1. madurella
6.2.2.1.2. pseudallescheria
6.2.2.1.3. exophiala
6.2.2.1.4. acremonium
6.2.2.1.5. acremonium
6.2.3. Sporotrichosis
6.2.3.1. rose gardener's disease
6.2.3.2. sporothrix schenckii: dimorphic ascomycetes
6.2.3.3. Fixed cutaneous sporotrichosis
6.2.3.4. Lympho-cutaneous sporotrichosis
6.2.4. Paranasal sinus phaeohyphomycosis
6.2.5. Cerebral phaeohyphomycosis

