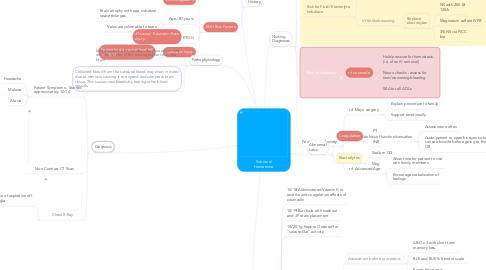
1. Patient History
1.1. Medical
1.1.1. Mitral Valve Prolapse
1.1.2. Atrial Fibrillation
1.1.2.1. Long-time coumadin patient
1.1.3. Prostate Cancer
1.2. Surgical
1.2.1. Mechanical Mitral Valve
1.2.2. Pacemaker
1.2.2.1. V-paced with underlying a-fib
1.3. SDH Risk Factors
1.3.1. Anti-coagulants
1.3.2. Age - 87 years
1.3.2.1. Brain atrophy with age, subdural space enlarges
1.3.2.2. Veins are vulnerable to tears
1.3.3. ETOH
1.3.3.1. Pt drinks "socially"
1.3.4. Traumatic Injury
1.3.4.1. Patient had a ground level fall on 10/14
2. Treatment Summary
2.1. 10/18 Administered Vitamin K to reverse anti-coagulation effects of coumadin
2.2. 10/19 Burr hole with washout and JP drain placement
2.3. 10/20 1g Keppra Ordered for "seizure-like" activity
2.4. 10/21 JP drain replaced and burrhole irrigated at the bedside
2.4.1. Assessment before procedure:
2.4.1.1. A&O x 3 with short term memory loss.
2.4.1.2. BLE and BUE 5/5 motor scale
2.4.1.3. Pupils Equal and Reactive
2.4.2. Re-assessment after procedure
2.4.2.1. Lethargic. Oriented to person/place only.
2.4.2.2. Slurred speech
2.4.2.3. Left sided weakness (1-2/5 on motor scale)
2.4.2.4. Left side facial droop
2.4.2.5. Follows commands well, but unable to open eyes
2.5. PICC placement
2.6. 10/21 Craniotomy with washout and 2 JP drains placed
3. Diagnosis
3.1. Patient Symptoms - Started approximately 10/14
3.1.1. Headache
3.1.2. Malaise
3.1.3. Ataxia
3.2. Non Contrast CT Scan
3.3. Chest X-Ray
3.3.1. Evidence of aspiration d/t dysphagia
4. Pathophysiology
4.1. #1 cause: Traumatic Brain Injury
4.2. blood accumulates between the dura mater and arachnoid layer of the meninges that cover the brain
4.3. Collected blood from the subdural bleed may draw in water due to osmosis, causing it to expand and compress brain tissue. This causes new bleeds by tearing other blood vessels.
5. Nursing Diagnoses
5.1. Impaired Cerebral Perfusion
5.1.1. r/t collection of blood and CSF in subdural space
5.1.1.1. 110 < SBP < 140
5.1.1.2. Seizure precautions
5.1.1.3. O2 via NC for SpO2 <94%
5.1.1.4. Strict I/O
5.1.1.5. Nuero checks Q2h
5.2. Risk for Fluid/ Electrolyte Imbalace
5.2.1. r/t NPO >48h
5.2.1.1. Strict I/O
5.2.1.1.1. Assisted with urinal while pt was able
5.2.1.1.2. Foley placed in OR
5.2.2. r/t Sodium wasting
5.2.2.1. Replace electrolytes
5.2.2.1.1. NS with 20K @ 120/h
5.2.2.1.2. Magnesium sulfate IVPB
5.2.2.1.3. 3% NS via PICC line
5.3. Risk for bleeding
5.3.1. r/t coumadin
5.3.1.1. Hold pressure for hemostasis (i.e. after IV removal)
5.3.1.2. Neuro checks - assess for new/worsening bleeding
5.3.1.3. SBA for all ADLs
5.4. Fear/ Death Anxiety
5.4.1. r/t Major surgery
5.4.1.1. Explain procedure to family
5.4.1.2. Support emotionally
5.4.2. r/t Sudden loss of function/sensation
5.4.2.1. Assess neuro often
5.4.2.2. Assist patient to open his eyes so he can see his wife before going to the OR
5.4.3. r/t Advanced Age
5.4.3.1. Allow time for patient to visit with family members
5.4.3.2. Encourage verbalization of feelings
6. Abnormal Labs
6.1. Coagulation
6.1.1. PT
6.1.2. INR
6.2. Electrolytes
6.2.1. Sodium 133
6.2.2. Mag

