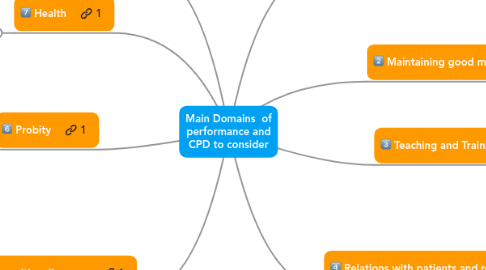
Main Domains of performance and CPD to consider
作者:Captain Walker
1. Appraisal
2. Health
2.1. 77. Register with a GP
2.2. 78. Immunisations and communicable disease
2.3. 79. Serious condition affecting judgement or performance
3. Probity
3.1. Being honest and trustworthy (paragraphs 56-59)
3.2. Providing and publishing information about your services (paragraphs 60-62)
3.3. Writing reports and CVs, giving evidence and signing documents (paragraphs 63-69)
3.4. Research (paragraphs 70-71)
3.5. Financial and commercial dealings (paragraphs 72-73)
3.6. Conflicts of interest (paragraphs 74-76)
4. Working relations with colleagues
4.1. Working in teams (paragraphs 41-42)
4.2. Conduct and performance of colleagues (paragraphs 43-45)
4.3. Respect for colleagues (paragraphs 46-47)
4.4. Arranging cover (paragraph 48)
4.5. Taking up and ending appointments (paragraph 49)
4.6. Sharing information with colleagues (paragraphs 50-53)
4.7. Delegation and referral (paragraphs 54-55)
5. Good clinical care
5.1. * Providing good clinical care (paragraphs 2-3)
5.2. * Supporting self-care (paragraph 4)
5.3. * Avoid treating those close to you (paragraph 5)
5.4. * Raising concerns about patient safety (paragraph 6)
5.5. * Decisions about access to medical care (paragraphs 7-10)
5.6. * Treatment in emergencies (paragraph 11)
6. Maintaining good medical practice
6.1. Keeping up to date para 12-13)
6.2. Maintaining and improving your performance (para 14)
7. Teaching and Training
7.1. About teaching, training, appraising and assessing doctors and students; developing appropriate skills and attitudes (para 15-19)
8. Relations with patients and relatives
8.1. * The doctor-patient partnership (paragraphs 20-21)
8.2. * Good communication (paragraphs 22-23)
8.3. * Children and young people (paragraphs 24-28)
8.4. * Relatives, carers and partners (paragraph 29)
8.5. * Being open and honest with patients if things go wrong (paragraphs 30-31)
8.6. * Maintaining trust in the profession (paragraphs 32-35)
8.7. * Consent (paragraph 36)
8.8. * Confidentiality (paragraph 37)
8.9. * Ending your professional relationship with a patient (paragraphs 38-40)