1. Pathogenesis
1.1. Autosomal dominant inheritence
1.1.1. Usually heterozygous
1.1.2. Heterozygous inheritance is often fatal to developing fetus
1.2. Progressive degeneration of neurons in brain
1.2.1. Late-stage disease usually leads to complete helplessness
1.2.1.1. Progressive loss of independence
1.2.1.2. Individual often remains aware of surroundings and retains ability to understand language
1.2.2. Death often occurs within 10 to 30 years of disease onset
1.2.2.1. Average age of death: 51-57
1.3. Death usually occurs secondary to:
1.3.1. Pneumonia
1.3.2. Cardiovascular disease
1.3.3. Other, lesser, causes include infection, fall-related injuries, dysphagia-related complications
2. Incidence and Prevalence
2.1. 4.1 to 8.4 per 100,000
2.1.1. Highest incidence in those of Western European descent
2.1.2. Lowest incidence in those of Japanese descent
2.1.3. Poor reporting on actual prevalence
2.2. Onset of symptoms usually develops between ages 35 to 44
2.3. Rare juvenile form of disease can occur as young as 20s
2.3.1. Juvenile Huntington disease is associated with different risk factors, diagnostics, symptoms, and treatments and is not covered in the scope of this project!
3. Risk Factors
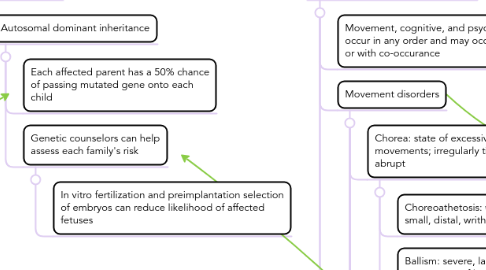
3.1. Autosomal dominant inheritance
3.1.1. Each affected parent has a 50% chance of passing mutated gene onto each child
3.1.2. Genetic counselors can help assess each family's risk
3.1.2.1. In vitro fertilization and preimplantation selection of embryos can reduce likelihood of affected fetuses
4. Clinical Manifestations
4.1. Movement, cognitive, and psychiatric disorders may occur in any order and may occur independently or with co-occurance
4.2. Movement disorders
4.2.1. Chorea: state of excessive, spontaneous movements; irregularly timed, randomly distributed, abrupt
4.2.1.1. Choreoathetosis: when paired with small, distal, writhing movements
4.2.1.2. Ballism: severe, larger, flinging movements of limbs
4.2.2. Bradykinesia and akinesia
4.2.2.1. Major source of loss of voluntary movement
4.2.3. Parkinsonian signs
4.2.3.1. Rigidity
4.2.3.2. Postural instability
4.2.4. Dystonia: sustained muscle contraction
4.2.4.1. Causes twisting, repetitive movements, abnormal postures
4.2.4.2. Sustained dystonia can lead to contractures, immobility, and skin breakdown
4.2.5. Eye movement disorders
4.2.5.1. Saccade: quick, simultaneous movement of both eyes, abruptly changing point of fixation
4.2.5.1.1. Slow and uncoordinated
4.2.5.1.2. Unable to inhibit saccades toward stimulus
4.2.6. Variable tendon reflexes
4.2.6.1. Flexor plantar reflex
4.2.7. Hyperkinesias
4.2.7.1. Tics
4.2.7.2. Myoclonus
4.3. Cognitive disorders
4.3.1. Rate of cognitive decline varies drastically
4.3.1.1. Some may retain cognitive ability throughout disease
4.3.2. Difficulty organizing thoughts
4.3.3. Tendency to get "stuck" on idea, thought, or action
4.3.4. Lack of impulse control
4.3.4.1. Outbursts
4.3.4.2. Acting without thinking
4.3.4.3. Sexual promiscuity
4.3.5. Lack of self awareness
4.3.6. Slowness in processing thoughts
4.3.7. Difficulty finding words
4.3.8. Difficulty learning new ideas
4.3.8.1. Associated with loss of previously learned skills or knowledge
4.4. Psychiatric disorders
4.4.1. Depression
4.4.1.1. Irritability
4.4.1.2. Social withdrawal
4.4.1.3. Insomnia
4.4.1.4. Fatigue or energy loss
4.4.1.5. Frequent thoughts of death or suicide
4.4.1.5.1. Increased risk of suicide
4.4.2. Obsessive-compulsive disorder
4.4.2.1. Recurrent or intrusive thoughts
4.4.2.2. Repetitive behaviors
4.4.3. Sleep disorders
4.4.3.1. Insomia
4.4.3.1.1. May be exacerbated by depression
4.4.4. Mania
4.4.4.1. Elevated mood and self esteem
4.4.4.2. Over-activity and impulsive behaviors
4.4.5. Bipolar disorder
4.4.5.1. Alternating periods of depression and mania
5. Diagnostics
5.1. Differentiation from chorea gravidarum, multiple sclerosis, and systemic lupus erythematosus may be required
5.2. Neurological examinations
5.2.1. Test motor symptoms
5.2.1.1. Reflexes
5.2.1.2. Muscle strength and tone
5.2.1.3. Coordination and balance
5.2.2. Test sensory symptoms
5.2.2.1. Sense of touch
5.2.2.2. Vision and eye movement
5.2.3. Test psychiatric symptoms
5.2.3.1. Mental status
5.2.3.2. General mood
5.3. Neuropsychological testing
5.3.1. Standardized tests to determine quality of:
5.3.1.1. Memory
5.3.1.2. Reasoning
5.3.1.3. Mental agility
5.3.1.4. Language function
5.3.1.5. Spatial reasoning
5.4. Psychiatric evaluation
5.4.1. Emotional state
5.4.2. Behavioral patterns
5.4.3. Quality of judgement
5.4.4. Coping skills
5.4.5. Signs of disordered thinking
5.4.6. Substance abuse
5.5. Brain imaging
5.5.1. MRI, CT, or PET scans
5.5.1.1. May be able to detect brain changes in more advanced diseases
5.6. Genetic testing
5.6.1. Confirmation of diagnosis
5.6.1.1. Beneficial if no family history is present or if family history has not been positively genetically confirmed
5.6.2. Genetic counseling may be provided prior to and following testing
5.6.2.1. Explain benefits and drawbacks to obtaining results
5.6.2.2. Explain inheritance patterns
5.6.2.3. Determine treatment plan
5.6.3. Predictive genetic testing
5.6.3.1. Can be given prior to onset of symptoms in presence of family history
5.6.3.2. Does not indicate age of onset or presence of symptoms
5.6.3.3. Genetic counseling may be given prior to and following testing
5.6.3.4. Some inherent risks
5.6.3.4.1. Increased insurance rates or denial of insurance
5.6.3.4.2. Difficulty obtaining future employment or potential loss of employment
5.6.3.4.3. Stress associated with fatal disease
6. Treatments
6.1. Important to note:
6.1.1. Nothing can prevent associated physical, mental, and behavioral decline
6.1.1.1. Medication can lessen movement and psychiatric symptoms
6.1.1.2. Using multiple interventions can help adaptation to changing abilities
6.1.2. Treatment evolves over course of disease as symptoms and severity change
6.1.3. Many medications used to treat particular symptoms may exacerbate others
6.2. Medication
6.2.1. Treat movement disorders
6.2.1.1. Tetrabenazine [Xenazine]
6.2.1.1.1. Suppresses involuntary chorea
6.2.1.1.2. Some negative side effects: worsening depression, drowsiness, nausea, restlessness
6.2.1.2. Antipsychotics
6.2.1.2.1. Unintended side effect of suppressing involuntary chorea
6.2.2. Treat psychiatric disorders
6.2.2.1. Antidepressants
6.2.2.1.1. Can help treat OCD and changing mood
6.2.2.2. Antipsychotics
6.2.2.2.1. Can help suppress violent outbursts, agitations, and other mood symptoms
6.2.2.3. Mood stabilizers
6.2.2.3.1. Treatment of bipolar and mania
6.3. Psychotherapy
6.3.1. May include social workers, psychiatrists, and psychologists
6.3.2. Managing behavioral problems
6.3.3. Coping strategies for progressing disease
6.3.4. Managing expectations of disease progression
6.3.5. Facilitating communication among family members
6.4. Speech therapy
6.4.1. Includes speech, eating, and swallowing
6.4.2. Use of communication devices as muscles deteriorate
6.4.3. Minimizing effects of dysphagia
6.4.3.1. Swallowing evaluations
6.4.3.2. Thickening liquids and changing food consistency
6.5. Physical therapy
6.5.1. Teaches appropriate and safe exercises to enhance strength, flexibility, balance, and coordination
6.5.1.1. Maintain mobility as long as possible
6.5.1.2. Reduce risk of falls
6.5.2. Teaches appropriate postures and uses of supports to maintain postures
6.5.2.1. May help lessen severity of some movement disorders
6.5.3. Teaches use of walkers, canes, and wheelchairs
6.5.3.1. Includes exercise regimens to adapt to new mobility
6.6. Occupational therapy
6.6.1. Help maintain quality of life, independence, and ADLs
6.6.2. Use of handrails and ramps at home
6.6.3. Use of assistive devices
6.6.3.1. Adaptive eating and drinking utensils
