1. Symptoms
1.1. The most common symptom is a quievering or fluttering heartbeat.
1.2. General Fatigue
1.3. Rapid and irregular heartbeat
1.4. Fluttering or "thumping" in the chest
1.5. Dizziness
1.6. Shortness of breath and anxiety
1.7. Weakness
1.8. Faintness or confusion
1.9. Fatigue when exercising
1.10. Sweating
1.11. Cheat pain or pressure
1.12. Sometimes people with AFib have no symptoms and their condition is only detectable upon physical examination.
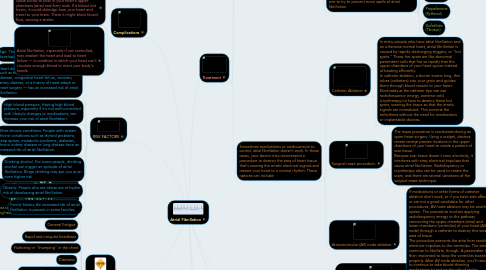
2. There are 3 different types of AFib that help the doctors classify the type of AFib problems.
3. RISK FACTORS
3.1. Age. The older you are, the greater your risk of developing atrial fibrillation.
3.2. Heart disease. Anyone with heart disease — such as heart valve problems, congenital heart disease, congestive heart failure, coronary artery disease, or a history of heart attack or heart surgery — has an increased risk of atrial fibrillation.
3.3. High blood pressure. Having high blood pressure, especially if it's not well-controlled with lifestyle changes or medications, can increase your risk of atrial fibrillation.
3.4. Other chronic conditions. People with certain chronic conditions such as thyroid problems, sleep apnea, metabolic syndrome, diabetes, chronic kidney disease or lung disease have an increased risk of atrial fibrillation.
3.5. Drinking alcohol. For some people, drinking alcohol can trigger an episode of atrial fibrillation. Binge drinking may put you at an even higher risk.
3.6. Obesity. People who are obese are at higher risk of developing atrial fibrillation.
3.7. Family history. An increased risk of atrial fibrillation is present in some families.
4. Complications
4.1. In atrial fibrillation, the chaotic rhythm may cause blood to pool in your heart's upper chambers (atria) and form clots. If a blood clot forms, it could dislodge from your heart and travel to your brain. There it might block blood flow, causing a stroke.
4.2. Atrial fibrillation, especially if not controlled, may weaken the heart and lead to heart failure — a condition in which your heart can't circulate enough blood to meet your body's needs.
5. What is Atrial Fibrillation (also called AFib or AF)?
5.1. Atrial fibrillation is an irregular and often rapid heart rate that can increase your risk of stroke, heart failure and other heart-related complications.
6. What happens during AFib?
7. Did you know?
7.1. 15-20 percent of people who have strokes also have this heart arrhythmia.
7.2. People with AFib have an increased stroke risk of about five percent per year.
7.3. AFib is the most common "serious" heart rhythm abnormality in people over the age of 65 years.
7.4. Many patients are unaware that AFib is a serious condition and only 33% of the patients that have it consider it to be serious.
8. Treatment
8.1. Generally, the treatment goals for atrial fibrillation are to: Reset the rhythm or control the rate and prevent blood clots
8.2. Resetting your heart's rhythm is a procedure called cardioversion. Cardioversion can be conducted in two ways.
8.2.1. Electrical cardioversion
8.2.1.1. After electrical cardioversion your doctor may prescribe anti-arrhythmic medications to help prevent future episodes of atrial fibrillation.
8.2.2. Cardioversion with drugs uses medications called anti-arrhythmics to help restore normal sinus rhythm. Depending on your heart condition, your doctor may recommend trying intravenous or oral medications to return your heart to normal rhythm. This is often done in the hospital with continuous monitoring of your heart rate. If your heart rhythm returns to normal, your doctor often will prescribe the same anti-arrhythmic medication or a similar one to try to prevent more spells of atrial fibrillation.
8.2.2.1. Medications may include:
8.2.2.2. Flecainide
8.2.2.3. Sotalol (Betapace, Sorine)
8.2.2.4. Although these drugs may help maintain a normal heart rhythm, they can cause side effects, including: dizziness, fatigue, and nausea.
8.2.2.5. Amiodarone (Cordarone, Pacerone)
8.2.2.6. Propafenone (Rythmol)
8.2.2.7. Dofetilide (Tikosyn)
8.3. Sometimes medications or cardioversion to control atrial fibrillation doesn't work. In those cases, your doctor may recommend a procedure to destroy the area of heart tissue that's causing the erratic electrical signals and restore your heart to a normal rhythm. These options can include:
8.3.1. Catheter Ablation
8.3.1.1. In many people who have atrial fibrillation and an otherwise normal heart, atrial fibrillation is caused by rapidly discharging triggers, or "hot spots." These hot spots are like abnormal pacemaker cells that fire so rapidly that the upper chambers of your heart quiver instead of beating efficiently. In catheter ablation, a doctor inserts long, thin tubes (catheters) into your groin and guides them through blood vessels to your heart. Electrodes at the catheter tips can use radiofrequency energy, extreme cold (cryotherapy) or heat to destroy these hot spots, scarring the tissue so that the erratic signals are normalized. This corrects the arrhythmia without the need for medications or implantable devices.
8.3.2. Surgical maze procedure.
8.3.2.1. The maze procedure is conducted during an open-heart surgery. Using a scalpel, doctors create several precise incisions in the upper chambers of your heart to create a pattern of scar tissue. Because scar tissue doesn't carry electricity, it interferes with stray electrical impulses that cause atrial fibrillation. Radiofrquency or cryotherapy also can be used to create the scars, and there are several variations of the surgical maze technique.
8.3.3. Atrioventricular (AV) node ablation
8.3.3.1. If medications or other forms of catheter ablation don't work, or if you have side effects or are not a good candidate for other procedures, AV node ablation may be another option. The procedure involves applying radiofrequency energy to the pathway connecting the upper chambers (atria) and lower chambers (ventricles) of your heart (AV node) through a catheter to destroy this small area of tissue. The procedure prevents the atria from sending electrical impulses to the ventricles. The atria continue to fibrillate, though. A pacemaker is then implanted to keep the ventricles beating properly. After AV node ablation, you'll need to continue to take blood-thinning medications to reduce the risk of stroke because your heart rhythm is still atrial fibrillation.
