1. SCID - Severe Combined ImmunoDeficiency Syndrom
1.1. Autosomal recessive inherited condition in Arabian foals - won't be passed on w/ responsible breeding
1.2. Pathogenesis:
1.2.1. 5 nucleotide loss causes frameshift mutation in DNA-dependent protein kinase which results in premature termination of the protein ---- deletion of 967 amino acids
1.2.2. This protein is necessary for rejoining of V,D,J gene segments following recombination which will prevent T & B cells from producing functional variable regions. Can't produce mature lymphocytes. Eliminates adaptive immune response
1.3. Clinical signs:
1.3.1. NK cells and granulocytes still functional
1.3.2. Foal protected via passive immunity until it runs out. Foals will succumb to infections
1.4. Diagnosis:
1.4.1. Antemortem: lymphopenia, lack of serum IgM (IgG could be materal - depends on test timing), PCR for 5 NT deletion
1.4.2. Postmortem: hypoplasia of lymphoid tissues, lack of lymphoid follicles and germinal centers; macrophages, NK cells, and fibroblasts will be present
2. Antigens / Immunogens
2.1. Any substance that can induce antibody generation / any substance that can be bound by specific immune responses (B or T cell receptors, MHC molecules
2.1.1. B cell receptors (antibodies) recognize peptides, sugars, lipids, nucleic acids, & hormones
2.1.2. Th & Tc cell receptors recognize only peptides that have been "processed" or degraded
2.1.2.1. γ/δ recognize lipids directly on pathogen surface
2.1.3. B cells have receptors to bind directly to the pathogen, T cells need to be presented with epitope by MHC molecule
2.2. GOOD antigen factors:
2.2.1. Size, complexity, stability, and foreignness
2.2.1.1. Proteins are excellent if >1000 Da
2.2.1.2. Simple polysaccharides are poor antigens, readily degraded in cells
2.2.1.3. Complex carbohydrates good especially if bound to proteins
2.2.1.4. Nucleic Acids poor ag unless bound to proteins
2.2.1.5. Lipids poor unless linked to proteins
2.2.2. Host Factors that affect potential immunogenicity:
2.2.2.1. Genetics - individuals vary
2.2.2.2. Age - immunity deficient in neonates and senescent individuals
2.2.2.3. Health Status
2.2.3. Environmental Factors:
2.2.3.1. Dose
2.2.3.2. Route of Exposure
2.2.3.3. Adjuvants
2.2.4. SQ>IP>IV>intragastric - slower clearance from SQ
2.3. ALLERGEN is antigen that induces an allergic reaction
2.4. EPITOPES are smaller parts of LG molecules that are bound by antibody or T cell receptor
2.4.1. each macromolecule contains many epitopes individually able to be bound by antibody/T cell receptors
2.4.2. MULTIVALENCY - epitopes are repeated several times
2.4.3. spatial arrangement of epitopes on single antigen can affect how antibodies bind
2.5. Tumor Antigens are presented on the surfaces of tumor cells by MHC class I and II molecules
2.6. HAPTENS are small molecules that are not normally immunogenic, but become antigens when linked to a carrier - forms a new epitope that is not big enough to be bound by antibody or T cell receptors
2.6.1. Ex: penicillin binds to albumin, Urushiol (poison ivy) is converted to a reactive compound that reacts with skin proteins
2.6.2. Haptens generate 3 types of antibodies: against carrier, against hapten, against new epitope of the hapten-carrier linkage
2.7. T independent Ag: are immunogenic enough that T cells aren't required to activate B cells for antibody production
2.7.1. Usually v. complex molecules with repeating epitopes
2.7.2. response can occur very early in an immune response & assist in host clearance of certain pathogens
2.8. Cross-reactivity: 1 epitope is similar enough to trigger a response against another epitope, even on v. different molecules. Results in specific immunity against apparently unrelated antigens
2.9. Antigen Exposure: Ag encountered in tissues are taken up by dendritic cells (& macrophages), moved to draining lymph nodes -- tend to elicit IgG antibodies Ag encountered on mucosal surfaces are taken up by specialized M cells or dendritic cells that extend thru epithelial lining -- tend to elicit AgA and IgE antibodies
2.9.1. Antigen Processing: degradation of proteins into peptides (epitopes that can bnd MHC for presentation to MHC molecules
2.9.1.1. Exogenous Ags are presented by MHC class II
2.9.1.2. Endogenous Ags are presented by MHC class I
2.9.2. Antigen Presentation: display of antigens as peptide fragments bound to MHC molecules on the surface of a cell
2.9.2.1. T cells have receptors that "test" Ags to determine if they are self-derived or foreign. Can't see whole Ag, only processed form
2.9.3. Antigen-Presenting Cells: highly specialized phagocytes that can display processed antigen as peptide fragments on the cell surface
2.9.4. Autoantigens: self antigens. Requires a host genetic predisposition for disease
2.10. Superantigens: secreted exotoxins that are highly mitogenic and stimulatory for T cells, don't require processing for presentation, work by crosslinking MHC and TCR to overstimulate T cells and drive hyperinflammation
3. Adaptive Immunity
3.1. Agglutination - uses multi-valency in order to limit the # of pathogens to deal with ---used in many dx tests
3.2. Humoral
3.2.1. Antibodies
3.2.1.1. IgM
3.2.1.2. IgG
3.2.1.3. IgE
3.2.1.4. IgA
3.2.1.5. Functions:
3.2.1.5.1. Neutralization - bind to protein on pathogen which is necessary for cellular infection, bind to toxins
3.2.1.5.2. Opsonization for phagocytosis - (IgG) Fab binds to pathogen, Fc binds to Fc receptor on phagocytic cell, allows phagocytic cell to pull the pathogen in and destroy it
3.2.1.5.3. Complement Fixation - (IgM) allows for activation of cell killing membrane attack complex
3.2.1.5.4. Antibody dependent cell-mediated cytotoxicity (ADCC) - ab binds to cell surface, NK cell recognizes ab thru Fc receptor and kills cell. Important again intracellular pathogens and cancer cells
3.3. Cellular
3.3.1. B Cells
3.3.1.1. IgM+Plasma Cell
3.3.1.2. Early B cell development:
3.3.1.3. Late Pro-B cell development
3.3.1.4. Large pre-B cell
3.3.1.5. Small pre-B cell
3.3.1.6. Immature B cell & Central Tolerance
3.3.1.7. Mature B Cell
3.3.1.8. Germinal Centers
3.3.1.9. Somatic Hypermutation (affinity maturation)
3.3.1.10. Class Switching (IgM -> IgG, IgA, or IgE)
3.3.1.10.1. Class switched Memory B cells
3.3.2. T Cells
3.3.2.1. Helper T cells
3.3.2.1.1. Th1
3.3.2.1.2. Th2
3.3.2.2. Cytotoxic T cells
3.3.2.3. Regulatory T cells
4. Failure of Passive Transfer
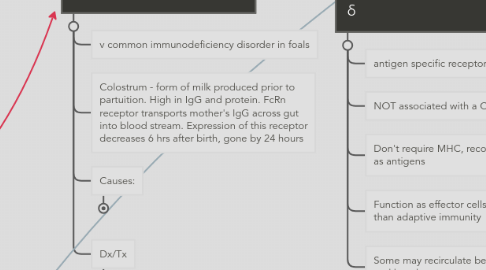
4.1. v common immunodeficiency disorder in foals
4.2. Colostrum - form of milk produced prior to partuition. High in IgG and protein. FcRn receptor transports mother's IgG across gut into blood stream. Expression of this receptor decreases 6 hrs after birth, gone by 24 hours
4.3. Causes:
4.3.1. Failure to produce colostrum because of a premature birth, of insufficient IgG levels due to young mother or mastits
4.3.2. Premature lactation, ingestion failure, absorption failure, neonatal infection (sepsis)
4.4. Dx/Tx
4.4.1. Determine IgG levels in colostrum and neonatal serum
4.4.2. W/in 1st 2 hours after birth: oral colostrum, oral serum or plasma, oral commercial colostrum
4.4.3. After 24 hours: IV or IP plasma, IV/IP/SQ commercial IgG
5. Alternate T cells - γ/ δ
5.1. antigen specific receptors
5.2. NOT associated with a CD4 or CD8
5.3. Don't require MHC, recognize lipids and carbs as antigens
5.4. Function as effector cells for innate immunity than adaptive immunity
5.5. Some may recirculate between tissues, blood, and lymph
6. Innate Immunity
6.1. Humoral
6.1.1. Complement
6.1.2. Cytokines
6.1.2.1. About:
6.1.2.1.1. small soluble proteins that are released by various cells in the body in response to an activating stimulus, induce a response thru binding to a specific receptor
6.1.2.1.2. regulate the intensity and duration of innate/adaptive immune responses, can function in autocrine/paracrine/endocrine
6.1.2.1.3. Influence action and biosynthesis of other cytokines (synergy & antagonism), Often work together to fully elicit a cellular response or immunological outcome
6.1.2.1.4. Cytokine receptors: expressed on various cell types v. specific for their ligand, are grouped into families based on signal transduction mechanisms or molecular structure
6.1.2.2. Growth Factors
6.1.2.2.1. Granulocyte Macrophage - Colony Stimulating Factor (GM-CSF)
6.1.2.2.2. Macrophage - Colony Simulating Factor (M-CSF)
6.1.2.2.3. Granulocyte - Colony Stimulating Factor (G-CSF
6.1.2.2.4. IL-7
6.1.2.3. Toll Like Receptors (TLRs)
6.1.2.3.1. important for sentinel cells (dendrititic and macrophages), bind to pathogen associated molecular patterns (PAMPs) and initiate cytokine production
6.1.2.4. Inflammatory Cytokines
6.1.2.4.1. IL-1β
6.1.2.4.2. TNF-α
6.1.2.4.3. IL - 6
6.1.2.5. Regulatory Cytokines
6.1.2.5.1. IL-10
6.1.2.5.2. TGF-β1
6.1.2.6. T & B cell associated
6.1.2.6.1. IL-2
6.1.2.6.2. IL-12
6.1.2.6.3. IL-17
6.1.2.6.4. IL-21
6.1.2.6.5. CD40L
6.1.2.7. Interferons
6.1.2.7.1. Type 2 (IFN-γ)
6.1.3. Chemokines
6.1.3.1. About:
6.1.3.1.1. Produced by phagocytic cells, T cells, endothelial cells, and fibroblasts
6.1.3.1.2. Regulate the migration of immune cells into inflammatory loci
6.1.3.1.3. Bind to specific receptors on the surface of specific immune cells
6.1.3.2. IL-8 (CXCL8)
6.1.3.3. IP-10 (interferon gamma produced protein) (CXCL10)
6.1.4. Antimicrobial peptides
6.1.4.1. Lactoferrin -[neutrophils and epithelial cells]- IRON BINDING, amphipathic w/affinity for bacterial & fungal lipids
6.1.4.2. Histatins -[Salivary glands]- Histidine-rich peptides w/affinity for fungal lipids
6.1.4.3. Lysozyme -[neutrophils, mø]- Cleaves bond between N-acetylglucosamine and N-acetylmuramic acid; Gram neg exclude this molecule from membrane
6.1.4.4. Cathelicidins -[neutrophils]- Family of membrane-binding proteins that disrupt the bacterial and fungal membrane
6.1.4.5. Defensins -[neutrophils, mø, epithelial cells]- Cationic, basic, pore-forming proteins that bind to bacterial and fungal membranes
6.2. Cellular
6.2.1. Monocytes
6.2.1.1. Macrophages
6.2.1.2. Dendritic Cells
6.2.2. NK Cells
6.2.3. Granulocytes
6.2.3.1. Mast Cells
6.2.3.2. Eosinophils
6.2.3.3. Basophils
6.2.3.4. Neutrophils
7. Acute Phase Response
7.1. Results in the production of C reactive protein and mannose binding lecting (MBL) by the liver which bind to pathogens and activate the complement cascade
8. Phagocytosis
8.1. process by which particles in the extracellular fluid are taken up by phagocytes
8.1.1. non-specific uptake
8.1.2. receptor mediated uptake -- result of opsonization
8.1.2.1. Complement receptors
8.1.2.2. acute phase protein receptors
8.1.2.3. toll-like receptors
8.1.2.4. scavenger receptors
8.1.2.5. Fc receptors
