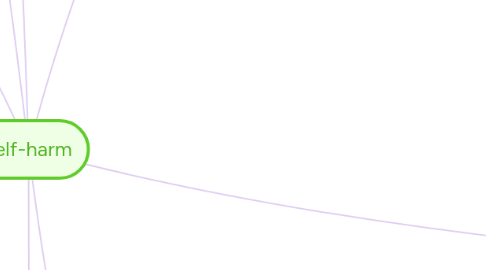
1. forms
1.1. cutting
1.1.1. most common
1.2. fist banging
1.3. eating disorders
1.3.1. bulimia
1.3.2. anorexia
1.4. scratching
1.5. burning
1.6. Hair pulling (trichotillomania)
1.7. substance abuse
1.7.1. overdosing
1.7.2. alcohol
1.7.3. drug
1.7.4. noxious substances
1.8. interfering with wound healing
2. Phenomenology
2.1. before self-harming
2.1.1. overwhelmed by emotions
2.1.1.1. tense
2.1.1.2. fearfull
2.1.1.3. isolation
2.1.1.4. dissociation
2.1.1.5. anxious
2.1.1.6. angry
2.1.2. emotion regulation
2.2. during self-harming
2.2.1. absence of pain
2.2.2. control
2.2.3. anger, tension and dissociation dissapears
2.3. after self-harming
2.3.1. positive emotions (common)
2.3.1.1. calm
2.3.1.2. satisfaction
2.3.1.3. relief
2.3.1.4. release
2.3.2. negative emotions (rare)
2.3.2.1. guilt
2.3.2.2. disgust
3. associated diagnoses
3.1. impulse disorder
3.1.1. similar to eating disorders or kleptomania
3.2. borderline personality disorder
3.3. depression
3.4. dissociative identity disorder
3.5. obsessive compulsive disorder
3.6. alcoholism
3.7. substance abuse
3.8. eating dissorders
3.9. schizophrenia
3.10. anxiety disorder
3.11. adjustment disorder
3.12. personality disorders
4. importance of intervention
4.1. correlated with antisocial behviour
4.2. associated with
4.2.1. increased suicide
4.2.2. sexual behaviours at high risk for HIV
4.2.3. physical illness and complaints
4.2.4. sexual dysfunction
4.2.5. symptoms of depression
4.2.6. psychiatric and emotional distress
5. risk factors (Gratz, 2003).
5.1. environmental risk factors
5.1.1. bullying
5.1.2. childhood separation and loss
5.1.3. psychological abuse
5.1.4. physical abuse
5.1.5. childhood sexual abuse
5.1.6. childhood trauma
5.1.7. familial risk factors
5.1.7.1. neglect
5.1.7.1.1. maternal emotional neglect
5.1.7.1.2. paternal emotional neglect
5.1.7.2. insecure attachment
5.1.7.2.1. insecure paternal attachment
5.1.7.3. parental deprivation
5.1.7.4. divorce
5.1.7.5. pathological family relations
5.1.7.6. emotional distancing
5.1.7.7. invalidating family environment
5.1.7.8. bereavement
5.2. individual risk factors
5.2.1. biological
5.2.1.1. Altered cortisol response
5.2.1.2. low serotogenic functioning
5.2.1.3. genetic predisposition
5.2.2. emotional dysregulation
5.2.2.1. emotional vulnerability
5.2.2.1.1. emotional reactivity: sensitivity to emotional stimuli
5.2.2.1.2. emotional intensity: extreme emotional reactions
5.2.2.1.3. inability to self-soothe
5.2.3. physiological
5.2.3.1. decreased psychophysiological response
5.2.4. dissasociation
5.3. population
5.3.1. adolescents
5.3.2. young adults
5.3.3. single females
5.3.4. asylum seekers, minority ethnic groups, people in institutional care or custody such as prisoners, sexual minorities, veterans and those bereaved by suicide
6. Background information
6.1. intention
6.1.1. non-suicidal
6.1.2. sexual
6.2. possible outcomes
6.2.1. under-employed and lower vocational achievement despite education
6.2.2. suicide
6.3. secret private and intimate act
6.4. onset: 13-14 years of age
6.5. 15%-20% lifetime prevalence
6.6. worldwide phenomenon, prevalence is similar
6.7. more common in psychiatric populations
6.8. contributing factors
6.8.1. genetic predisposition and psychiatric, psychological, familial, social, and cultural factors
6.8.2. media and contagion is increasingly important
7. most influential factos
8. intrapersonal functions
8.1. emotion regulating functions
8.1.1. affect regulation
8.1.1.1. express self hate
8.1.1.2. acute negative affect before DSH
8.1.1.3. decreased negative affect and relief after DSH
8.1.1.4. intent: to alleviate negative affect
8.1.1.5. outcome: negative affect and arousal are reduced with DSH
8.1.1.6. regulate overwhelming affect
8.1.1.6.1. sense of control
8.1.1.7. 'need to express or control anger, anxiety, or pain that cannot be expressed verbally or through other means'
8.1.2. anti-dissociation
8.1.2.1. to end
8.1.2.1.1. depersonalisation
8.1.2.1.2. dissociation
8.1.2.2. maintain sense of self
8.1.2.3. conectedness to the world
8.1.3. self-punishment
8.1.4. externalize emotional pain
8.1.4.1. making it physical and tangible therefore easier to understand and less abstract
8.1.4.2. physical evidence of emotional pain
8.1.4.3. making their emotions real, justified and tolerable
8.1.4.4. validates the emotion
8.1.5. escape
8.1.5.1. forget worries, fears, emotional pain
8.1.6. relaxation
8.1.6.1. relieve anxiety
8.1.6.2. release tension
8.1.6.3. release anger
8.1.6.4. reduce stress
8.1.7. sense of security, safety & protection.
8.1.8. empower
8.1.8.1. prove themselves they can cope with that pain
8.1.9. anti-suicide drive model (psychoanalysis)
8.1.9.1. replace or avoid suicide, compromise between drives to live and die
8.2. relieve unpleasant thoughts and feelings
8.2.1. relieve feelings of guilt, loneliness, alienation, self-hatred, and depression
8.2.2. stop racing thoughts
8.2.2.1. self reinforcement
8.2.2.1.1. SH decreases tension and dissociation through affect regulation function
8.2.3. end flashbacks bad memories
8.3. sensation-seeking
8.3.1. generate excitment
8.3.1.1. endorphines
8.4. sexual drive model (psychoanalysis)
8.4.1. 'Self-mutilation stems from conflicts over sexuality, menarche, and menstruation'
9. Dialectical Behaviour Therapy (DBT) (Brodsky, & Stanley, 2013)
9.1. combines cognitive behavioural and supportive intervention
9.1.1. including behavioral skill training, contingency management, cognitive modification, and exposure to emotional cues
9.1.2. supportive techniques such as reflection, empathy, and acceptance
9.1.3. group therapy focusing on the development of interpersonal skills, skills aimed at tolerating distress, and emotion regulation skills
9.2. particularly effective with adolescents
9.3. outcomes
9.3.1. enables them by providing tools to achieve the lives they want to lead
9.3.2. learn to
9.3.2.1. explore emotions
9.3.2.2. regulate and respond to emotions
9.3.3. significant reduction in the frequency of self-harm after 12 months of DBT
9.4. 5 core skills
9.4.1. mindfulness
9.4.1.1. experience emotion without SH
9.4.2. distress tolerance
9.4.2.1. alternatives to SH
9.4.2.2. how to deal with impulse
9.4.3. emotion regulation
9.4.3.1. understand and control painful feelings
9.4.4. the middle path
9.4.4.1. minimise extreem thoughts, not everything is black and white, search for middle ground
9.4.5. interpersonal effectiveness
9.4.5.1. how to meet their needs
9.4.5.2. promote self-respect behaviours
9.5. targets: pupils who have difficulty engaging and remaining in treatments
9.6. dialectic
9.6.1. accept and validate SHs as they are
9.6.2. help SHs to change
9.7. addresses emotion regulation, impulse control and problem-solving skills
9.8. 4 stages
9.8.1. stage 1: stabilising the patient and achieving behavioural control
9.8.1.1. decrease SH behaviours
9.8.1.2. decrease behaviours that interfere with therapy
9.8.1.3. decrease behaviours that interfere with quality of life
9.8.1.4. increase behavioural skills
9.8.2. stage 2: address past traumas
9.8.3. stage 3: develop self-esteem and managing day to day problems
9.8.4. stage 4: promote individual capacity to develop and have new experiences
9.9. assumptions
9.9.1. Pupils are doing the best they can
9.9.2. pupils want to improve
9.9.3. pupils need to do better try harder and have motivation to change
9.9.4. pupils may not have caused their problems but need to solve them
9.9.5. current life is unbearable
9.9.6. pupils cannot fail in therapy
9.9.7. BPD clinicians need support
9.10. most integrated and effective approach
10. negative behaviour replacement strategy
10.1. muscular pain through exercise
10.2. the release of chemicals through exercise can reinforce this healthier behaviour
11. functions (Suyemoto, 1998)
11.1. intergroup functions
11.1.1. competition with peers
11.1.2. social status
11.1.2.1. admiration
11.1.2.2. ability to endure pain
11.1.2.3. strength
11.1.2.4. courage
11.2. interpersonal functions
11.2.1. environmental
11.2.1.1. interpersonal-influence
11.2.1.1.1. communicate
11.2.1.2. 'Self-mutilation creates environmental responses that are reinforcing to the individual while simultaneously serving the needs of the environment by sublimating and expressing inexpressible and threatening conflicts and taking responsibility for them'
11.2.1.3. social contagion
11.2.1.3.1. modelling
11.2.1.3.2. vicarious reinforcement
11.2.2. boundaries (self-psychology)
11.2.2.1. maintain sense of self in relation to others, set boundaries between the self and others. Not to loose their identity
12. social and behavioural learning theory (intergroup level of analysis)
12.1. family relationships
12.2. deflect attention from dysfunctional environment
12.3. behaviours are maintained through
12.3.1. operant conditioning
12.3.2. classical conditioning
12.4. intermittent reinforcement schedules make behaviours difficult to erradicate
12.5. learning principles provide a non-judgemental explanation of behaviours
12.6. social contagion (Rosen, Walsh, & Rode, 1990)
12.7. modeling, imitation, and identification (Simpson & Porter, 1981)
12.7.1. learn from parents
12.7.2. self-care through self-injury
12.8. behaviours reinforced by (Offer and Barglow, 1960)
12.8.1. attention and concern from others
12.8.2. social status
13. psychoanalytic and object relations developmental theory (interpersonal)
13.1. explains prevalence in adolescents
13.1.1. differentiation from the mother
13.1.2. need to separate from infantile love objects
13.1.2.1. extreme defensive manouvers against infatile love objects
13.1.2.1.1. reversed affect
13.1.2.1.2. intolerable for the ego
13.2. individuals may display
13.2.1. inability to express emotion and conflict between self and others
13.2.2. perceived abandonment
13.2.2.1. early object relations
13.2.2.1.1. results in
13.2.2.1.2. due to
13.2.3. difficulty verbalizing emotions and needs, especially anger and feelings around loss
13.2.3.1. express overwhelming emotions
13.2.3.1.1. difficulty with verbal expression
13.2.3.1.2. lack of symbolising function
13.2.3.1.3. SH because language cannot be used to distance the individual from emotions and regulate affect
13.2.3.1.4. SH = primative evocative symbol
13.2.3.1.5. 'However, SH fails to communicate the information in which the primitive feeling is embedded or help the self-mutilator obtain mastery over the emotion through the use of symbolic communication. '
13.2.3.2. express and contain affect and need
13.3. linked to self psychology
13.4. rooted in ego psychology
14. Psychodynamic therapy (Levy, Yeomans, & Diamond, 2007)
14.1. patients learn to
14.1.1. accept emotions
14.1.2. express feelings verbally
14.1.3. tolerate intense emotions
14.1.4. make unconscious impulses conscious
14.1.5. alternative ways to control emotions
14.1.6. alternative ways of interacting with others
14.1.7. evoke soothing representations
14.2. most commonly used in SH
14.3. a good relationship with therapist
14.3.1. the best approach is to combine education, identification with the therapist, and a balance between permissiveness and limit setting
14.3.2. individual becomes more open honest and trusting
14.3.2.1. decreasing interpersonal difficulties
14.3.2.2. increasing self-esteem
14.3.2.3. reducing self-harm
14.3.2.4. sense of safety
14.3.3. technical neutrality
14.3.3.1. non-judgmental,
14.3.3.2. non-critical stance
14.4. most common improvement outcomes
14.4.1. an increased ability to cope with feelings, especially sexual and angry feelings
14.4.2. increased verbal expression of feelings
14.4.3. learning to use more constructive means to channel impulses
14.4.4. control of psychotic delusions
14.4.5. improved social adjustment
15. Neurobiology of SH (Groschwitz, & Plener, 2012)
15.1. Behaviour reinforcement
15.1.1. SH releases
15.1.1.1. endorphines
15.1.1.1.1. pleasurable feelings
15.1.1.1.2. pain killers
15.1.1.2. enkephalins
15.1.1.2.1. euphoria
15.1.1.2.2. stress relief
15.2. Neurotransmitter differences
15.2.1. decreased serotonin activity found in SHs
15.2.2. decreased serotonin
15.2.2.1. lack of constraint
15.2.2.1.1. difficult to resist the impulse to SH
15.2.2.2. impulsive behaviour
15.2.2.3. higher levels of stress
15.2.2.4. influences mood and aggression
15.2.2.5. reduced mean frontal binding index
15.3. Trauma
15.3.1. systematic abuse causes stress response system to become under responsive to stress chemicals
15.3.1.1. altered structure and chemistry of brain
15.3.1.1.1. constant state of fear and anxiety
15.3.1.1.2. altered stress response system
15.3.1.2. Stress chemicals: Epinephrine, Dopamine and Norephrine.
15.3.1.2.1. abused girls have been found to have higher levels of these chemicals
15.3.1.2.2. these chemical may trigger hyper arousal state of anxiety in SH
15.3.1.2.3. these hormones are released through flashbacks and nightmares engraining the traumatic memory
15.3.2. Catecholamines are released in the brain during sexual abuse.
15.4. addiction
15.4.1. Endogenous opioids (petrochemicals)
15.4.1.1. released when in danger or injured
15.4.1.1.1. act as pain killers
15.4.1.2. traumatic thoughts trigger segregation of natural opiates (endorphine response)
15.4.1.2.1. analgesic effect
15.4.1.3. addiction to opioids and their calming effect is created
15.4.1.4. absence of stress or traumatic triggers
15.4.1.4.1. opiate withdrawal and cravings
15.4.1.5. through SH opiates are released
15.4.1.5.1. lack of pain when SH
15.4.1.5.2. cravings are reduced
15.5. Genetic predisposition for high physical, cognitive and emotional reactivity
16. non-competitive exercise therapy (Berger, & Owen, 1988)
16.1. effects are comparable to antidepressants
16.2. stress reduction
16.3. mood enhancement
16.4. similar set of chemicals are released during exercise than during SH
16.4.1. reduce cravings
16.4.2. endogenous opioids
16.4.2.1. animal studies report addiction to exercise due to the release of opioids
16.4.3. serotonin

