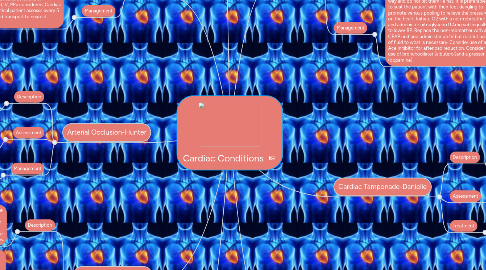
1. Arterial Occlusion-Hunter
1.1. Description
1.1.1. Arterial occlusion is an occlusion of arterial blood flow due to trauma, thrombosis, tumor, embolus, or idiopathic means. Emboli are the most common cause.
1.2. Assessment
1.2.1. Symptoms can include loose of sensation distal to the occlusion. Pain can occur during periods of exertion and is lessened with rested. Skin may be cool and cyanotic distal to the occlusion as well.
1.3. Management
1.3.1. Medical diagnosis is required for accurate treatment. High flow O2 and rapid transport to an appropriate facility. Morphine can be given for pain.
2. HTN Emergencies-Jim
2.1. Description
2.1.1. Hypertension is a chronic disease in which the blood pressure levels are continuously elevated. Sometimes these levels become life threatening. A hypertensive emergency is characterized by an increase in blood pressure accompanied by end- or target organ changes.
2.2. Assessment
2.2.1. Begin with the ABCs and any life threats. Conduct the history and physical assessment. These patients usually have nausea/vomiting, blurred vision, shortness of breath, chest pain, epistaxis, and vertigo. The patient could also have altered mental status, be unresponsive, or be seizing. Determine the patient's medication compliance status.
2.3. Management
2.3.1. Place the patient in a position of comfort. Provide airway and ventilatory support if needed. Gain IV access but di=o not prolong scene time. If the patient is a pregnant female place her on her left side. Place patient on the cardiac monitor and treat any arrhythmias found.
3. Cardiogenic Shock-Danielle
3.1. Description
3.1.1. Cardiogenic Shock is a condition in which your heart suddenly cant pump enough blood to meet the body's needs. The condition is most often caused by a severe heart attack.
3.2. Assessment
3.2.1. Rapid breathing, severe shortness of breath, tachycardia, change in LOC, weak pulse, sweating, pale skin, cold hands.
3.3. Treatment
3.3.1. High flow O2, IV, cardiac monitoring, medications to increase blood pressure and improve heart function such as Epi, Dopamine. If there is a heart rhythm disturbance, urgent treatment may be needed such as electrical shock therapy.
4. PE-Chris
4.1. Description
4.1.1. Pulmonary Embolism is a complete blockage of arterial blood flow to the lungs causing inadequate perfusion.
4.2. Assessment
4.2.1. shortness of breath,chest pain, light headedness, low oxygen, dry cough.
4.3. Management
4.3.1. Hi flow 15L NRB with considerations of intubation if needed,IV, PPv considered, Cardiac monitor 12 lead, Critical patient assesss every 5 minutes enroute and transport to nearest approriate facillity.
5. Aortic Aneurism-Hunter
5.1. Description
5.1.1. Aortic aneurism is a diatation or weakness in the aorta
5.2. Assessment
5.2.1. Aneurisms usually grow slowly without symptoms. A pulsing sensation may be felt near the navel area. The Patient may describe the pain as "shearing". Pain in the back, belly, or sign may indicate an impending rupture.
5.3. Treatment
5.3.1. Reducing the blood pressure may help prevent a rupture. Labetalol 20mg can be given via slow IV push over 2 minutes to reduce BP. High flow O2 and rapid transport to an appropriate facility.
6. CHF -Jim
6.1. Description
6.1.1. Congestive Heart Failure is a syndrome in which the heart's ability to meet the demands of the body is compromised. The cardiac output is no longer sufficient to meet the demands placed on it. CHF is divided into left sided failure and right sided failure. Left ventricular failure is when the heart fails as an effective forward pump and fluid backs up into the left ventricle. Right ventricular failure is when the heart fails as a forward pump and fluid backs up in the venous circulation.
6.2. Assessment
6.2.1. Begin with the ABCs and possible life threats assessments. Check the skin CTCs. Gain the patient's chief complaints. Use the OPQRST pneumonic to gather the patient's description of symptoms. Patient with this condition will display shortness of breath and clear or pink tinged sputum and mild chest pain.
6.3. Management
6.3.1. Do not have the patient exert themselves in any way and do not let them lie flat. It is preferable to seat the patient with their feet dangling to promote venous pooling to relieve the pressure on the heart. Initiate O2 with a non-rebreather and administer nitroglycerin 0.4mg sublingually to lower BP. Replace the non-rebreather with a CPAP unit and administer an IV but restrict use of fluid to what is necessary. Consider use of an Ace inhibitor for afterload reduction. Consider use of bronchodilator (albuterol)and a pressor (dopamine).
7. Cardiac Tamponade-Danielle
7.1. Description
7.1.1. Cardiac Tamponade is pressure on the heart that occurs when blood or fluid builds up in the space between the heart muscle and the outer covering of the sac.
7.2. Assessment
7.2.1. low blood pressure, weakness, chest pain radiating to the neck shoulders or back. trouble breathing, taking breaths, discomfort thats relieved by sitting or leaning for forward. change in LOC. Beck's Triad- increased heart rate, muffled heart tones, JVD hypotension.
7.3. Treatment
7.3.1. Provide O2, IV, fluid bolus, cardiac monitor, pericardiocentensis.
8. ACS-Chris
8.1. Description
8.1.1. Acute coronary syndrome- a sign or symptom accurs spontaneously due to the blockage or decrease in coronary artery blow flow to the heart muscle.
8.2. Assessment
8.2.1. presents with chest pain, shortness of breath, radiating pain to right arm, chest pressure,sweating.
8.3. Management
8.3.1. Hi flow o2 15L NRB,325 mg aspirin IV, po,0.4 mg nitro if BP is above 100 sytolic and no known vasodilating drugs have been taking prior to administaraion, cardiac monitor 12 lead, critical patient assess every 5 minutes in route to nearest facillity.
