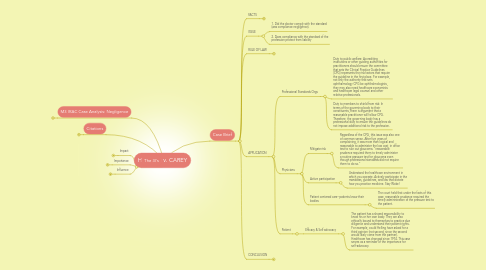
1. M3 IRAC Case Analysis: Negligence
1.1. Morrison P. HELLING and Barbara Helling, his wife v. Thomas F. CAREY and Robert C. Laughlin Supreme Court of Washington, En Banc. No. 42775. March 14, 1974
2. Citations
2.1. Journal of the American Academy of Psychiatry and the Law Online Commentary: Helling v. Carey Caveat Medicus http://jaapl.org/content/jaapl/36/3/306.full.pdf
2.2. Justia US Law Helling v. Carey
2.3. Law School Heretic Helling v. Carey: Courts establishing medical malpractice standards Helling v. Carey: Courts establishing medical malpractice standards
2.4. Law School Briefs: Helling v. Carey case brief
2.5. http://bit.ly/2vZrG0U
3. The 3I's
3.1. Impact
3.1.1. The courts decide! Clinical practice Guidelines may be the Bible for practitioners, but at the end of the day, the court gets to tell the doctor how to do their job. This is similar to health insurance! Insurers get to tell doctors and patients what care they need and what medicine they can or cannot have under their plan.
3.2. Importance
3.2.1. Reasonable practitioner does not automatically protect from strict liability. A doctor can follow all of the standards of care, and still be liable.
3.3. Influence
3.3.1. How practitioners treat patients: In this case, a simple test could have prevented glaucoma. Doctors must also weigh the costs vs. risks. This was a simple, low cost test. Therefore, the benefit of the test outweighs the risk of not administering (blindness)
3.3.2. Alternate influence: Futile medical care. A recent survey of 2,000 doctors, conducted by a JHU research team notes that futile care is driven by fear of malpractice. Since the percentage of patients diagnosed with glaucoma under 40 is low compared to the number over 40, there is argument that the test is futile.
4. Case Brief
4.1. FACTS
4.1.1. Parties
4.1.1.1. Barbara Helling, patient, age 32
4.1.1.2. Dr. Thomas F. Carey and Dr. Robert C. Laughlin, private practice ophthalmology partners.
4.1.2. What Happend
4.1.2.1. Patient complained of vision problems and was prescribed contact lenses. Patient continued to have problems over a 5 year period, after which she was diagnosed with glaucoma.
4.1.2.2. Despite continued vision complaints, the doctors failed to conduct a simple screening test for glaucoma, since the probability of disease was so low for patients age.
4.1.3. Procedural History
4.1.3.1. A). HELLING files suit for failure to timely administer a glaucoma test B). Trial & appellate court rule in favor of doctors (they followed standard of care). C). HELLING appeals
4.2. ISSUE
4.2.1. 1. Did the doctor comply with the standard (was compliance negligence).
4.2.2. 2. Does compliance with the standard of the profession protect from liability
4.3. RULE OF LAW
4.3.1. Reasonably prudent specialist
4.4. APPLICATION
4.4.1. Professional Standards Orgs
4.4.1.1. Duty to public welfare: Accrediting institutions or other guiding authorities for practitioners should ensure the committee that sets the Clinical Practice Guidelines (CPG) represents the risk factors that require the guideline in the first place. For example, not only the authority that sets ophthalmology CPG be ophthalmologists, they may also need healthcare economists and healthcare legal counsel and other relative professionals.
4.4.1.2. Duty to members to shield from risk: In terms of the governing body to their constituents, there is argument that a reasonable practitioner will follow CPG. Therefore, the governing body has a professional duty to ensure the guidelines do not impose additional risk to the profession.
4.4.2. Physicians
4.4.2.1. Mitigate risk
4.4.2.1.1. Regardless of the CPG, this issue was also one of common sense. After five years of complaining, it was more than logical and reasonable to administer the low cost, in office test to rule out glaucoma. "reasonable prudence required them to timely administer a routine pressure test for glaucoma even though professional standards did not require them to do so."
4.4.2.2. Active participation
4.4.2.2.1. Understand the healthcare environment in which you operate. Actively participate in the mandates, guidelines, and law that dictate how you practice medicine. Stay Woke!
4.4.2.3. Patient centered care--patients know their bodies
4.4.2.3.1. The court held that under the facts of this case, reasonable prudence required the timely administration of the pressure test to the patient.
4.4.3. Patient
4.4.3.1. Efficacy & Self advocacy
4.4.3.1.1. The patient has a shared responsibility to know his or her own body. They are also ethically bound to themselves to practice due diligence and understand their patient rights. For example, could Helling have asked for a third opinion (not second, since the second would likely come from the partner). Healthcare has changed since 1974. This case serves as a reminder of the importance for self-advocacy.
4.5. CONCLUSION
4.5.1. Judgement reversed. ophthalmologist were liable and negligent.
