1. Screening
1.1. Colonoscopy
1.1.1. Age 50-74: stool test every 2 years, colonoscopy 1 time.
1.1.2. After age 74: unless first screening, do not continue colonoscopy
1.1.3. Age 50 (with risk): colonoscopy, re-screen in 10 years, re-screen in 5 years if Hx of polyps
1.2. Annual Fecal Occult Blood Test
1.2.1. Every Year
1.3. CT colonography
1.3.1. Every 5 years
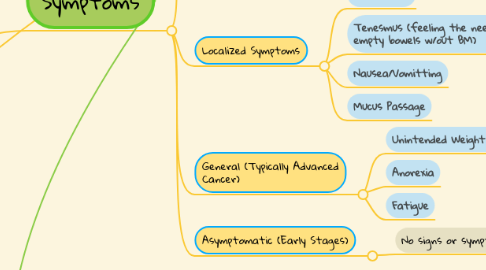
2. Symptoms
2.1. Common Symptoms
2.1.1. Rectal Bleeding
2.1.2. Abdominal Pain
2.1.3. Changes in Bowel Habits (diarrhea/constipation longer than 3 days)
2.1.4. Hematochezia (Passage of blood through anus, often with stool).
2.2. Localized Symptoms
2.2.1. Rectal Pain
2.2.2. Tenesmus (feeling the need to empty bowels w/out BM)
2.2.3. Nausea/Vomitting
2.2.4. Mucus Passage
2.3. General (Typically Advanced Cancer)
2.3.1. Unintended Weight Loss
2.3.2. Anorexia
2.3.3. Fatigue
2.4. Asymptomatic (Early Stages)
2.4.1. No signs or symptoms
3. Screening Results
3.1. Positive Colonoscopy
3.1.1. When doctor finds polyps or abnormal tissue
3.1.2. Polyps are not cancerous, but they can be pre-cancerous
3.1.3. Polyps found are removed (biopsy) to test for cancerous cells
3.1.3.1. Dx made based on lab results of biopsy
3.2. Positive Blood Test/ CT
3.2.1. Blood in the stool
3.2.2. Unusual growths on CT
4. Staging
4.1. Stage I
4.1.1. Tumor Invades submucosa. Can invade as far as muscularis propria and remain stage I
4.1.2. No Regional node metastasis
4.1.3. No Distant metastasis
4.2. Stage II
4.2.1. Invades muscularis propria into pericolorectal tissue OR Invades through visceral peritoneum OR Invades/adheres to adjacent organs or structures
4.2.2. No regional node metastasis
4.2.3. No distant metastasis
4.3. Stage III
4.3.1. Minimum 1, up to as many as 7 regional nodes positive
4.3.2. OR: No regional nodes positive, but tumor deposits in subserosa, mesentery, or nonperitonealized pericolic/perirectal/mesorectal tissue
4.4. Stage IV
4.4.1. Metastasis to distant organs or sites
4.4.2. Peritoneal metastasis may be identified. Any metastasis in peritoneal area = stage IV.
5. Treatment
5.1. Factors Affecting Treatment
5.1.1. Location of tumor
5.1.2. First Episode vs. reoccurrence
5.1.3. Stage
5.1.4. General Patient Health
5.1.5. Patient Preference
5.2. Choosing Treatment By Stage
5.2.1. Stage I
5.2.1.1. Surgery is the most common intervention. Due to no spread of the tumor follow-up/prior chemotherapy/radiation unlikely
5.2.2. Stage II
5.2.2.1. Surgery recommended
5.2.2.2. Chemotherapy post-surgical for prevention. Applied when patient is at high-risk of reoccurrence
5.2.2.2.1. Cancer has been found in nearby lymph nodes
5.2.2.2.2. Cancer was found at the edge of the removed tissue (sone left behind)
5.2.2.2.3. Cancer was obstructive
5.2.2.2.4. Cancer caused a perforation
5.2.2.3. Chemotherapy combined with radiation. This is used for individuals who are too weak for surgery
5.2.3. Stage III
5.2.3.1. Surgery to remove cancer from rectum/colon & lymph nodes
5.2.3.2. Chemotherapy standard as follow-up
5.2.3.3. Chemotherapy/radiation as treatment for those not healthy enough for surgery
5.2.4. Stage IV
5.2.4.1. Surgery unlikely unless only metastasized to a couple new places
5.2.4.2. Depending on tumor size, chemotherapy before surgery to shrink tumor
5.2.4.3. If non-curable (terminal), surgery will be avoided and chemotherapy may be implemented to improve quality/length of life
5.2.4.3.1. Surgery would only occur to remove tumor if it was found to be obstructive
5.2.4.4. Radiation therapy. Used to alleviate symptoms and pain. More prominent in rectal cancer than colon cancer.
6. Treatment Complications
6.1. Surgical Complications
6.1.1. Anastomotic Leak
6.1.1.1. A leak at a point of surgical joining
6.1.1.2. Presents as abdominal pain and fever
6.1.1.3. Patient drains purulent/bile drainage
6.1.1.4. CT scan would show extra-luminal contents in lumen.
6.1.2. Anastomotic Hemorrhage
6.1.2.1. Bleeding, very early posoperative
6.1.2.2. Warrants re-operation
6.1.3. Ileus
6.1.3.1. Lack of movement in GI post-surgery
6.1.3.2. Ileus can lead to intestinal obstruction
6.1.4. Gastrointestinal fistula
6.1.4.1. GI tract opened up, gastric fluid seeps into the intestines. Surrounding organs can be affected.
6.2. Radiotherapy Complications
6.2.1. Nausea, vomitting
6.2.2. Diarrhea
6.2.3. Loss of appetite
6.2.4. Small-bowel damage
6.3. Chemotherapy Complications
6.3.1. Skin reactions
6.3.2. Neurotoxicity
6.3.3. Diarrhea
6.3.4. Neutropenia (low WBCs, immunocompromised).
7. Post-Surgical Screening
7.1. Physical exam every 3-6 months for 2 years, then every 6 months for 3 years.
7.2. Carcinoembryonic antigen testing every 3 to 6 months for 2 years, then every 6 months for 3 years.
7.2.1. This is for high risk patients for reoccurrence.
7.3. CT of chest, abdomen, pelvis every 6 to 12 months for 5 years
7.4. Colonoscopy in 1 year. If Dx without colonoscopy, preform within 3 months. Repeat in 3 and 5 years.
8. Surgeries
8.1. Local Excision/local resection
8.1.1. Removes abnormal tissue
8.1.2. Stage 0/I surgery
8.1.3. Could be done with endoscopy, especially for rectal cancer
8.2. Bowel Resection
8.2.1. Most common surgery for colorectal CA
8.2.2. removes either part of rectum/intestine
8.2.3. Removal of nearby lymph nodes
8.3. Colostomy/ileostomy
8.3.1. Stoma is created either from the colon or ileum.
8.3.1.1. Permanent: Ileostomy/colostomy may be permanent in the case where surgery compromises the colon/rectum to a point where it will not be able to be operational again.
8.3.1.2. Temporary: An ileostomy/colostomy may be temporary in a case where the colon/rectum needs time to heal after surgery, and once everything has been given time to heal the patient can have a ileostomy/colostomy reversal surgery
8.4. Metastatic surgery
8.4.1. Wherever the metastasis are, only used if there are very few metastasis.
9. Chemotherapy
9.1. Chemotherapy drugs includeAdrucil, Xeloda, Eloxatin, Camptosar, Tomudex, Lonsurf
10. Radiation
10.1. For Rectal Cancer
10.1.1. Frequently given before surgery, often combined with chemotherapy. Makes surgery much easier for surgeons.
10.1.2. Used with or without chemo if a person is not healthy enough for surgery
10.2. Types
10.2.1. External-beam, radiation therapy (EBRT)
10.2.1.1. Most common for rectal cancer
10.2.1.2. Radiation focused from a machine outside the body
10.2.2. Internal Radiation therapy (brachytherapy)
10.2.2.1. More research needed
10.2.2.2. Radioactive source is put inside the rectum, next to the tumor
10.2.2.3. Benefit: reaches the rectum without having to pass through the skin and other tissues. Less damage
10.2.3. Radioembolization
10.2.3.1. Tiny glass/resin beads filled with radioactive isotope yttrium Y-90 placed in blood vessels feeding the tumor
11. Ostomy Management
11.1. Wound Care Consult
11.1.1. Nurses are trained and prepared to provide ostomy care and patient teaching, however the wound care nurse is the specialist
11.1.1.1. Assessments
11.1.1.1.1. Stoma is pink & moist
11.1.1.1.2. Monitoring output volume/consistency
11.1.1.1.3. Skin around stoma isn't irritated
11.1.1.1.4. Stoma sticks out of skin, hasn't widened/retreated back into body
11.1.1.1.5. Absence of bleeding
11.1.1.1.6. Monitoring patient for fever
11.1.2. Even though nurses can provide patient teaching, wound-care nurses are specialists in ostomy management and care
11.1.2.1. The wound care nurse will teach the patient:
11.1.2.1.1. About ho change their specific ostomy. Cutting the materials to the right size, cleaning with gauze and water, and when to apply protective powder for irritation.
11.1.2.1.2. About different types of ostomy bags
11.1.2.1.3. About the signs of ostomy infection
11.1.2.2. The wound care nurse will allow the patient to ask questions
11.1.2.2.1. About the changes of day to day life living with an ostomy
11.1.2.2.2. About how often it needs to be changed/burped
11.1.2.2.3. About resources for adjustment to living with an ostomy
