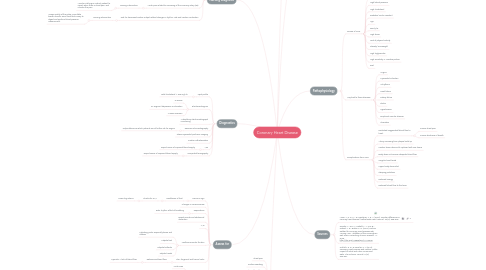
1. Nursing Diagnosis
1.1. Altered tissue perfusion related to narrowing of the coronary artery(ies) associated with atherosclerosis
1.1.1. Nursing intervention
1.1.1.1. Monitor consciousness, inspect skin extremities for cyanosis, cold skin and peripheral pulse degradation, and monitor intake and output.
1.2. Activity intolerance related to imbalance between oxygen supply and demand associated with necrotic tissue
1.2.1. Nursing intervention
1.2.1.1. Record heart rhythm, blood pressure and pule before and after activity. Also instruct patient to rest before and after activity
1.3. Acute pain related to narrowing of the coronary artery (ies)
1.3.1. Nursing intervention
1.3.1.1. Monitor vital signs, instruct patient to report when there is chest pain, and monitor the pain
1.4. Risk for decreased cardiac output related changes in rhythm, rate and cardiac conduction
1.4.1. Nursing intervention
1.4.1.1. Assess quality of the pulse, auscultate breath sounds, serve food that is easy to digest and perform blood pressure measurement
2. Assess for
2.1. Homan's Sign
2.1.1. Dosiflexion of foot
2.1.1.1. Checks for DVT
2.1.1.1.1. Lower leg edema
2.2. Changes in consciousness
2.3. Respirations
2.3.1. Rate, rhythm, effort of breathing
2.4. Bowel sounds and abdominal distention
2.5. JVD
2.6. Xanthomas under the skin
2.6.1. Palpating joints, especially knees and elbows
2.6.2. Palpate feet
2.6.3. Palpate buttocks
2.6.4. Palpate hands
2.7. Skin, fingernail and toenail color
2.7.1. Determines blood flow
2.7.1.1. Cyanotic = lack of blood flow
2.8. Heart sounds
2.8.1. Aortic area
2.8.2. Pulmonic area
2.8.3. Erb's point
2.8.4. Tricuspid area
2.8.5. Mitral area
3. Diagnostics
3.1. Lipid profile
3.1.1. Total cholesterol > 200 mg/ dL
3.2. Electrocardiogram
3.2.1. Q waves
3.2.2. ST segment depression or elevation
3.2.3. T wave inversion
3.3. Ambulatory electrocardiograph monitoring
3.4. Exercise echocardiography
3.4.1. Helps determine which patients are at further risk for angina
3.5. Stress myocardial perfusion imaging
3.6. Cardiac catheterization
3.7. MRI
3.7.1. Depict zones of impaired blood supply
3.8. Computed tomography
3.8.1. Depict zones of impaired blood supply
4. S&S
4.1. Chest pain
4.2. Profuse sweating
4.3. Labored breathing
4.4. Pallor
4.5. Fatigue
4.6. Activity intolerance
4.7. Dizziness
4.8. Palpitations
4.9. Lower extremity swelling
4.10. Weakness
4.11. Xanthoma
4.12. Xanthelasma
4.13. Coughing
5. System
5.1. Cardiovascular
6. Pathophysiology
6.1. Causes of CHD
6.1.1. Smoking cigarettes
6.1.2. High blood pressure
6.1.3. High cholesterol
6.1.4. Diabetes/ insulin resistant
6.1.5. Age
6.1.6. Family hx
6.1.7. High stress
6.1.8. Lack of physical activity
6.1.9. Obesity/ overweight
6.1.10. High triglycerides
6.1.11. High sensitivity C- reactive protein
6.1.12. Diet
6.2. May lead to these diseases
6.2.1. Angina
6.2.2. Myocardial infarction
6.2.3. Arrhythmia
6.2.4. Heart failure
6.2.5. Kidney failure
6.2.6. Stroke
6.2.7. Hypertension
6.2.8. Peripheral vascular disease
6.2.9. Ulceration
6.3. Complications from CHD
6.3.1. Restricted oxygenated blood flow to heart
6.3.1.1. Causes chest pain
6.3.1.2. Causes shortness of breath
6.3.2. Artery narrowing from plaque build up
6.3.3. Cardiac tissue dies and it replaced with scar tissue
6.3.4. Body does not receive adequate blood flow
6.3.5. Irregular heart beats
6.3.6. Upper body discomfort
6.3.7. Sleeping problems
6.3.8. Reduced energy
6.3.9. Reduced blood flow to the brain
